Empowers decision-makers to improve health outcomes
for communities they serve through cutting-edge AI, drivers of health data, and geospatial analytics.
Largest drivers of health dataset with data on 335M+ people in the US
Individual-level data with 10 years of history on 1,700+ data variables
Insight-generating predictive models driven by AI to reveal actionable economic, health, and lifestyle insights
Reveal deep insights about
population health
HealthPrism provides a unique opportunity to examine large populations, using advanced analytics techniques to derive insights that are often not possible using publicly available data.
Helping to Solve Your Challenges
Identify unique sub-populations
HealthPrism can identify drivers of health that could influence health outcomes and can pinpoint programs and interventions to lower risks.
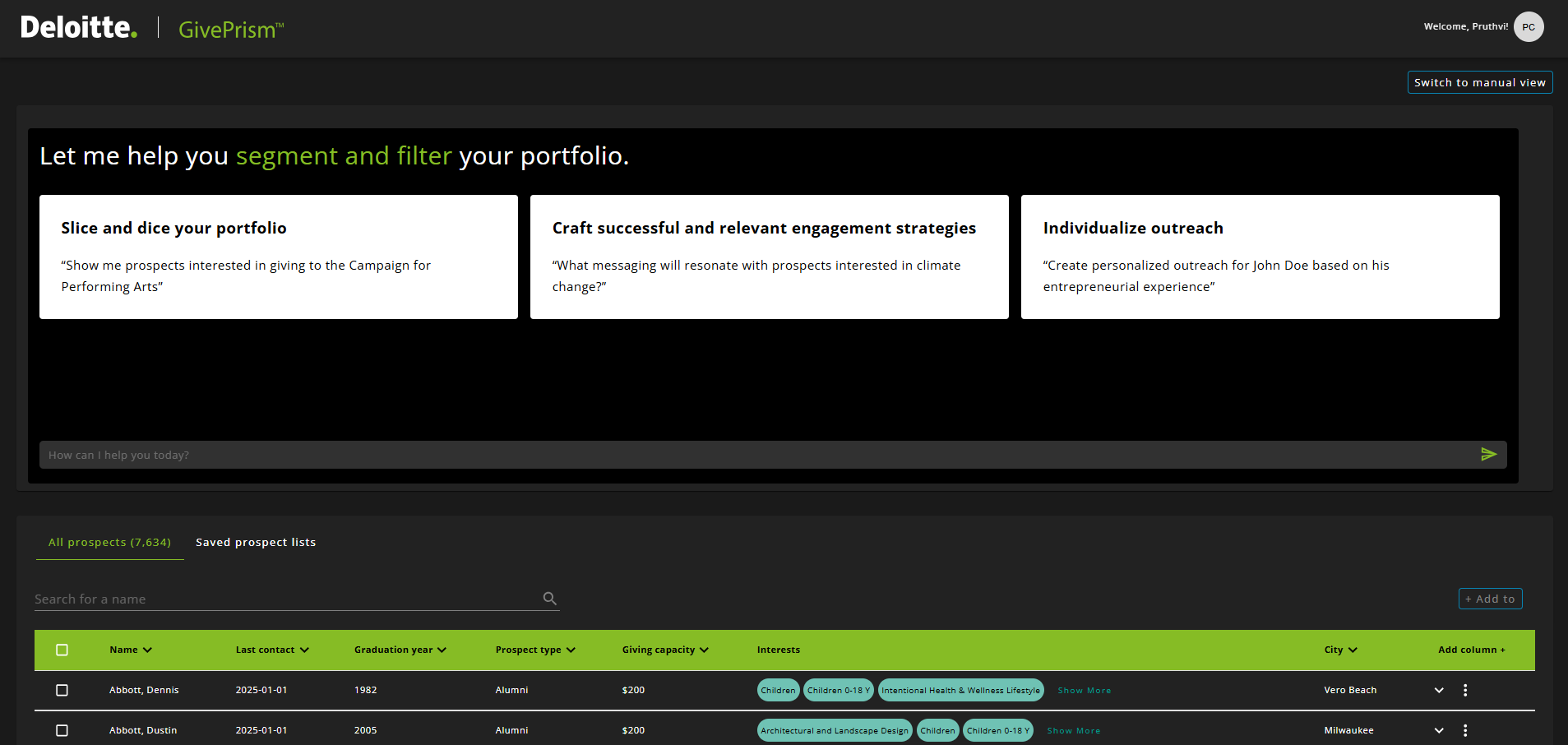
Activate the community
HealthPrism can inform micro-tailored outreach campaigns by identifying optimal messaging strategies and modes of outreach.
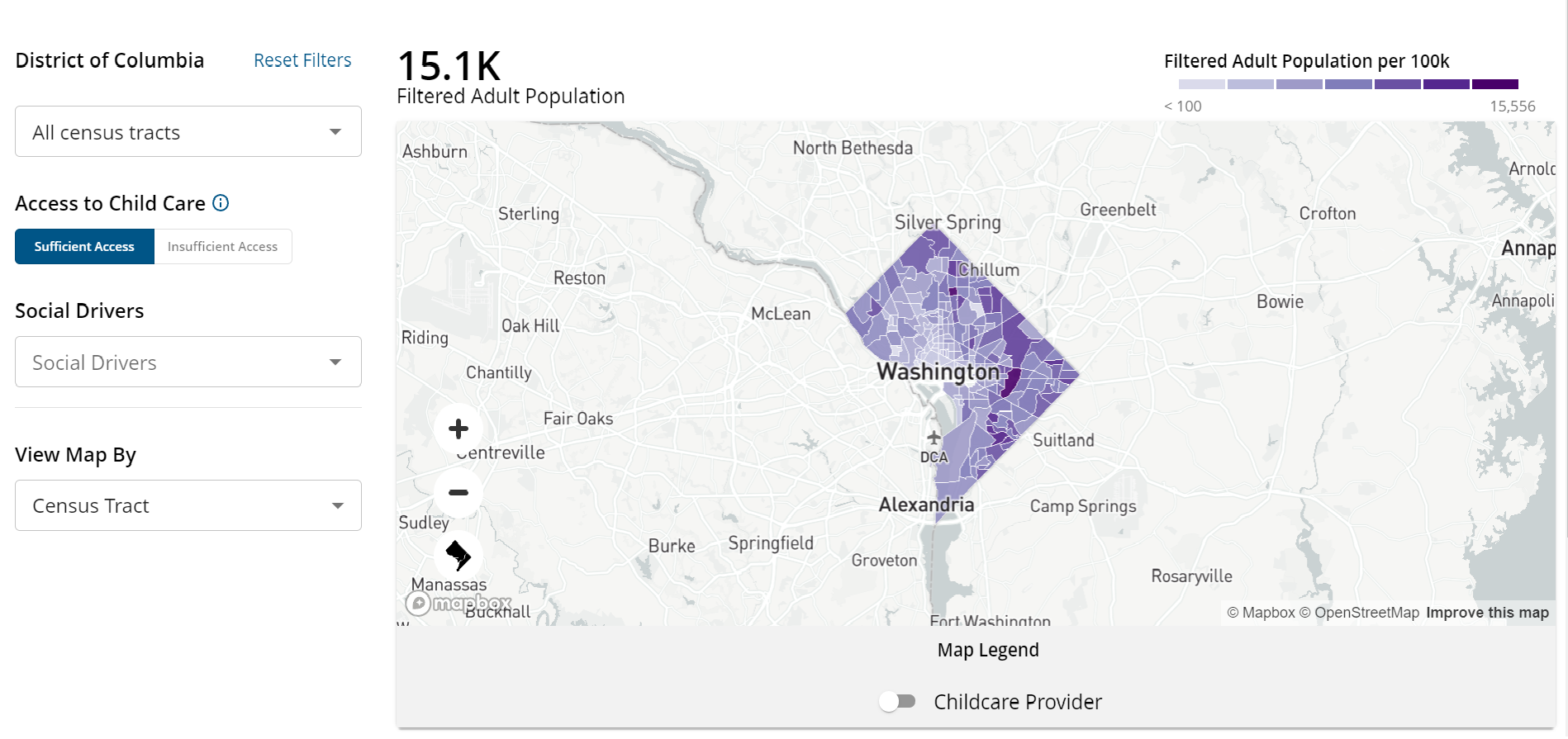
Guide resource allocation
HealthPrism can find care deserts and populations facing barriers to healthy outcomes to drive deployment of resources down to the neighborhood-level.
Measure effectiveness
HealthPrism can evaluate program and intervention efficacy using 10 years of longitudinal data, gauging population changes over time.
Get to know HealthPrism
Explore a wide variety of policy challenges impacting the populations you serve
Despite ongoing community interventions and prevention efforts, both fatal and non-fatal drug overdoses continue to rise. States and community leaders can take several actions to address this crisis.
New and innovative strategies to address drug overdoses are needed to curb this national issue.
Use the map to find places in the US that could most benefit from educational campaigns, naloxone distribution sites, and substance use disorder treatment centers.
This dashboard was created using HealthPrism data.
Who can benefit from HealthPrism?
State Departments of Health
State Departments of Medicaid
Federal Health Agencies
Health Non-profit Organizations
Commercial Healthcare Organizations
Any organization addressing health outcomes
HealthPrism Success Stories
Addressing Health Disparities in Underserved Communities
Federal Health
Federal Health Agency
HealthPrism has played a pivotal role in a Federal Health Agency’s effort to mitigate hypertension risks among populations in underserved regions across the United States.
With the power of detailed analytics, leaders used HealthPrism to facilitate the effective use of grant-funding aimed at reducing hypertension illness, deaths, and health disparities in these vulnerable communities.
Leaders used HealthPrism to facilitate effective use of grant funding
March of Dimes
March of Dimes Maternity Care Deserts Dashboard
HealthPrism empowers public-sector and private-sector leaders and other stakeholders to combat the maternal health crisis by providing data-driven insights revealing intricate connections between maternity care deserts and disparities in income, and health outcomes among women of childbearing age.
HealthPrism provided data-driven insights to reveal intricate connections in maternity care deserts
Mid-Atlantic State Department of Health
Mid-Atlantic State Department of Health Behavioral Segmentation for Preventative Health Outreach
HealthPrism reveals crucial insights into health access and behaviors shaped by environmental, and economic factors. By leveraging machine learning and expertise in behavioral science and public health, HealthPrism segmented this state’s population into 15 unique personas to enable micro-tailored outreach.
HealthPrism segmented this state's population into 15 unique personas to enable micro-tailored outreach
Frequently Asked Questions
Where do you get the data?
HealthPrism data comes from over 50 large commercially available consumer marketing data sets as well as publicly available data from the CDC and the US Census.
What is different about this data?
HealthPrism helps resolve data gaps that are common in publicly available data sources, such as underreporting of unhoused populations, by compiling data from over 50 data sources and using predictive modeling methods to accurately cover data gaps.
HealthPrism gives the ability to look at multiple data variables at once, enabling users to segment broad populations by multiple variables to find unique sub-populations.
Because HealthPrism has individual-level data, it can easily be integrated with your data at any level of aggregation.
How do you build predictive models?
HealthPrism leverages semi-supervised machine learning (ML) methods to train explainable predictive models. HealthPrism generates modeling datasets that represent the US population with respect to legally protected groups. HealthPrism extend bias checks further to include representation across income groups and the Rural-Urban Continuum Codes. Additionally, each variable input into a model is examined for its distribution with respect to age, income, the rural-urban continuum, and other demographic factors to help ensure that they do not act as a proxy for any of those variables. This bias awareness and examination can also influence the strategy for model selection where only explainable and interpretable models are used to train and predict risk.
How do you protect the data?
HealthPrism is committed to maintaining the privacy of personal data, protecting user data and maintaining transparency with strict controls around data usage:
Is this real-time data?
HealthPrism data reflects predictive estimates based on multiple demographic and consumer marketing data sources. HealthPrism updates underlying data and risk estimates on a regular basis (typically every one to two months, depending on the source). In other words, the data in this dashboard is updated on a consistently recurring basis as opposed to a real-time basis.
How does HealthPrism address gaps in race and ethnicity data?
Populations that suffer disproportionately high rates of death and disease such as racially and ethnically diverse populations, people with disabilities, and rural populations are underrepresented in some health research, and their status as part of those groups is often not recorded in critical health care records. This lack of data is a serious barrier to advancing equity.
Race and ethnicity data are particularly essential to understanding and improving health equity. However, race and ethnicity data on much of the US population is missing from many health-related data sets. Race and ethnicity are often poorly documented in commercial health records like insurance claims. Additionally, gaps in data and outdated information in public data sources like the US Census can hinder meaningful insights into race and ethnicity. These gaps can prevent recognition of very real health disparities and delay action to improve equity.
To enable meaningful action on health equity, HealthPrism uses predictive models based on the Bayesian Improved Surname Geocoding Method (BISG) to fill the gaps in missing race and ethnicity data (this method is used by government agencies like the Virginia Department of Health). In addition, HealthPrism uses other data science methods to improve race and ethnicity predictive model accuracy. HealthPrism includes self-reported race where such data is available and displays predicted race where no self-reported data is available.
Contact Us
HealthPrism's Lead Staff
Managing Director, Deloitte Consulting LLP
Chris Stehno
Principal, Deloitte Consulting LLP
Sean Conlin
Vice President, Product Strategy
Raaj Parekh

Senior Manager, Deloitte Consulting LLP
Mike Daggitt
More Solutions